Medical practices spend an average of two business days a week per physician to comply with health plans’ inefficient and overused prior-authorization (PA) protocols. One-third of practices employ staffers who spend every second of their working hours on PA requests and follow-ups.
Like sands through the hourglass, so are the days of prior authorization.
These figures come from the responses to a 27-question, web-based AMA survey administered to 1,000 American physicians who provide at least 20 hours of patient care per week. The toll of prior authorization is rising, they said.
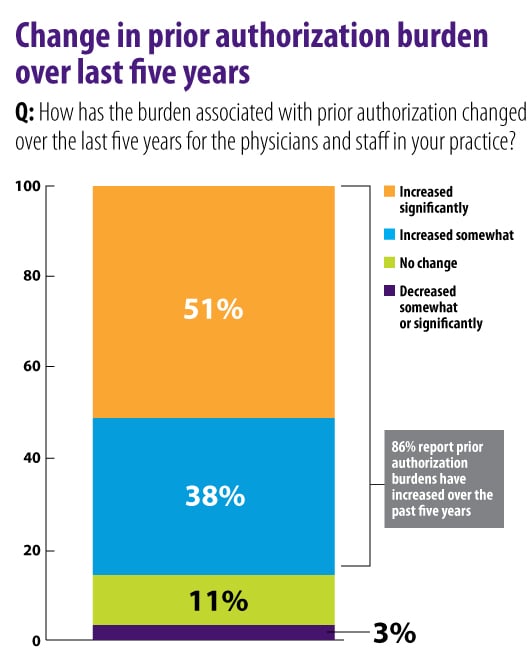
Nearly 90 percent of the physicians reported that the administrative burden related to PA requests has risen in the last five years, with most saying it has “increased significantly.”
Jack Resneck Jr., MD, a health policy expert and professor of dermatology at the University of California, San Francisco, said the survey results reflect the dismaying reality that now delays doctors’ orders for even routine prescriptions.
“Physicians have, for many years, expected to face prior-authorization hurdles for a few new or unusually expensive medications or tests. But, more recently, insurers have rapidly added PA requirements to more and more treatments,” Dr. Resneck, chair-elect of the AMA Board of Trustees, told AMA Wire®. “This survey demonstrates the increasing burden.”
On average, a medical practice will complete 29.1 PA requests per physician per week that take 14.6 hours to process. About half of the requests are for medical services, while the other half are for prescriptions, the survey found.
“In my own practice, I now get insurer rejections or PA demands for a majority of the prescriptions I write each day—even for many generic medications that have existed for decades,” Dr. Resneck said. “For many conditions I see, even when there are several treatment options, I increasingly run into plans where every single one of those choices requires a PA.”
Dr. Resneck’s experience is the new normal.
Seventy-nine percent of the physicians surveyed reported that they sometimes, often or always are required to repeat the PA process for prescription medications when a patient is stabilized on a treatment regimen for a chronic condition.
“While most of these PA requests ultimately get approved, the time my staff and I spend filling out lengthy forms and calling health plans to appeal is substantial—and those are hours I am unable to spend face to face with patients,” Dr. Resneck said. “My practice has several medical assistants who spend countless hours helping our physicians on PAs each week.”
Unmerry-go-round
Almost two-thirds of physicians reported having to wait at least one business day for the decision from a health plan on a PA request. Nearly one in four physicians wait an average of three to five days, and 7 percent wait more than five days, the survey found.
This corresponds with the 92 percent of physicians who said PA sometimes, often or always delays patients’ access to necessary care.
“Physicians face additional frustrations when initial PA requests are rejected, with health plans often replying with recommendations for alternatives that make no sense given a patient’s condition,” Dr. Resneck said.
“This leads to resubmissions and additional phone calls to further explain why a patient needs a particular treatment or why the suggested alternative is completely inappropriate,” he added. “The health-plan employees on the other end of these interactions sometimes don’t know anything about the medication I’m requesting, and I find myself explaining diseases and treatments to them all too often.”
Payers agree to work on reform
Some relief appears to be coming. Earlier this year, the AMA joined with other stakeholders—including the insurance industry trade group America’s Health Insurance Plans and the Blue Cross Blue Shield Association—to issue a consensus statement that announced their commitment to improving the prior-authorization process.
More recently, the AMA and Anthem agreed to work together on a number of issues to improve patients’ access to timely, high quality and affordable care. Streamlining or eliminating low-value PA requirements is among the issues the collaboration will focus on.
“I’m so glad that some insurers have recently come to the table to work with physicians on ways to reduce this burden and improve access for patients,” Dr. Resneck said. “We’re working with them to reduce the number of treatments subjected to prior authorization, exempt those physicians who demonstrate high approval rates, improve transparency of requirements, protect patients who are already on treatment, and make submission of PA requests easier.”
Other AMA resources on prior authorization include model legislation and instructional videos on how to reduce administrative burdens by using electronic PA processes that are integrated into a physicians’ electronic health record workflow.
Through the Physicians Grassroots Network and the Patients Action Network, the AMA is giving physicians and patients a way to share their experiences with prior authorization and add their voices to advocacy for reform.