Medicare Advantage (MA) can enable innovation that aligns the values of patients and physicians and allows doctors to feel better about the work they’re doing—and reduce burnout in the process, according to two physician experts who have been practicing within the capitated value-based care model.
As health care in general, and Medicare in particular, move away from fee-for-service payments and toward value-based care, “physicians on the front line will need effective pathways that actually work for them as well as their patients,” said Jennifer Caudle, MD, host of an AMA-sponsored ReachMD podcast, “The Realities of Medicare Advantage: Perspectives on Physician & Patient Outcomes,” which is part of a special series of programs on the potential on value-based care.
As opposed to Medicare fee for service, MA pays physicians a per member, per month capitated fee that may go up or down “based on the acuity of the patients that you have in your panel,” said Barbara Spivak, MD, president and CEO of the Mount Auburn Cambridge Independent Practice Association (IPA), in Massachusetts.
MA’s capitated model allows practices to invest in care teams and technology while giving physicians more time to spend with their patients said Griffin Myers, MD, chief medical officer with Oak Street Health, a network of primary care practices headquartered in Chicago with locations in seven states. Oak Street Health was one of 22 health care organizations to earn AMA Joy in Medicine™ Recognition for outstanding efforts to address the systemic causes of physician burnout in areas such as assessment, leadership, teamwork and practice-environment efficiency.
Drs. Spivak and Myers shared their comments as part of the podcast.
Balancing less choice, more risk
Dr. Spivak, co-chair of the AMA Integrated Physician Practice Section’s Policy Development Committee, noted that MA’s drawbacks include a more limited network for patients. Also, MA requires most of the financial risk to fall on providers such as hospitals, specialty practices, primary care physicians or some combination of all three.
Practices that enter into MA contracts should also have a reinsurance program to cover years in which a “confluence” of patients may require care that is more expensive than anticipated.
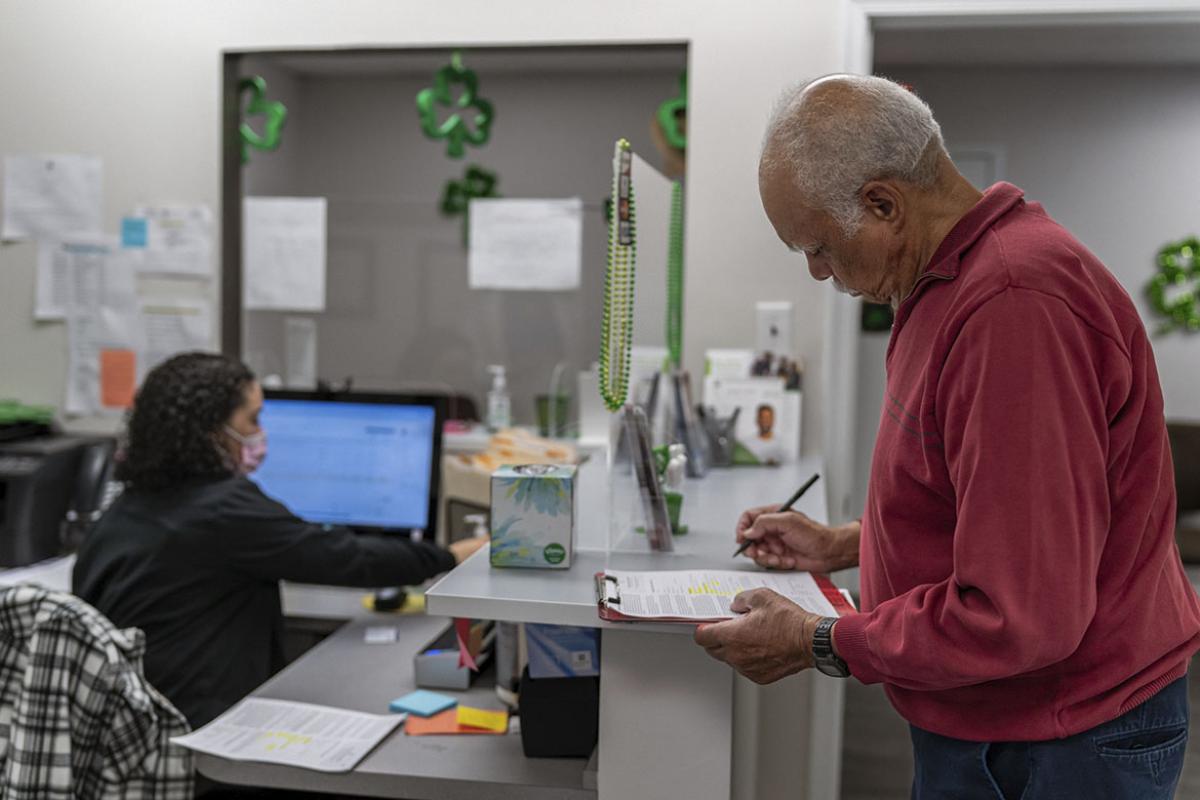
But, Dr. Spivak said, these aspects of MA are worth it because physicians are provided with significant amounts of data that helps them deliver better care. Also, the capitation payment allows for investment in additional staff and services patients appreciate such as rides to visits and nutritious food delivered to their homes. Social workers also work to link patients with resources available in their communities.
Higher patient engagement
“Patients really like it,” Dr. Spivak added. “They become very attached to the people who are working with them to get them better care. Patients are more engaged in their own care and actually do better just by virtue of having more people helping them.”
Dr. Myers agreed, noting that the capitated payments help support each Oak Street primary care physician with a team consisting of a medical assistant, nurse, full-time scribe, care manager and behavioral health specialist. Based on its MA contracts, Oak Street has built a system where that team takes care of about 500 people who have nine appointments annually, with 5% of patients who require more services are seen 19 times a year.
In addition, they can also provide, when needed, telepsychiatry, podiatry and in-house social services. The highest acuity patients can also get in-home primary care, Dr. Myers said.
Using a combination of personnel and technology applications, Oak Street has been able to achieve 15% reductions in hospital readmissions, he added.
Results “worth celebrating”
For physicians considering entering into an MA contract, Dr. Spivak recommends taking the time to organize systems and being willing to invest in the technology infrastructure, noting that the rewards will pay off in terms of physician, patient and staff satisfaction.
Dr. Spivak added that operating as an IPA allows for a central office that handles coding and other administrative burdens as care is delivered locally.
Dr. Myers said that Medicare Advantage is a “crucial component” to improving equity and access for older populations and its success in doing so is “worth celebrating,” especially in how it can help develop “new payment mechanisms that drive us to the results we want.”
The AMA has payment resources developed by experts and early innovators in new payment models to help physicians adopt reforms