Access to a physician with specialty or subspecialty training moves the needle on improving patient outcomes in the physical medicine and rehabilitation field—and telehealth is a means for providing needed access to specialty care.
That was the take-home message from Mary Alexis Laccarino, MD, a physiatrist with specialty in neurological rehabilitation, who gave an assessment of the evidence on the beneficial use of telehealth in concussion treatment and management during an AMA Future of Health Immersion Program webinar (registration required) on telehealth in physical medicine and rehabilitation.
The AMA hosted the webinar in collaboration with the American Academy of Physical Medicine and Rehabilitation (AAPM&R), and panelists discussed the findings of a white paper published in PM&R: The Journal of Injury, Function and Rehabilitation that assesses the evidence regarding telehealth’s effectiveness in the different domains of physical medicine and rehabilitation.
The paper summarizes how telehealth is best used in the specialty while highlighting knowledge deficits and technological limitations and identifying new opportunities for PM&R translational research.
“Evidence does support that it's feasible to do telehealth as much of care is provided with clinical interview, use of self-assessment tools and involvement of education in return to activity,” said Dr. Laccarino, an assistant professor at Harvard Medical School’s Spaulding Rehabilitation Hospital.
Supporting telehealth is an essential component of the AMA Recovery Plan for America’s Physicians.
Telehealth is critical to the future of health care, which is why the AMA continues to lead the charge to aggressively expand telehealth policy, research and resources to ensure physician practice sustainability and fair payment.
Remote knee rehab works
Telerehabilitation can be delivered through audiovisual or audio-only communication, but can also involve virtual-reality devices, gaming therapy as well as instruments to measure body movements.
Some of the strongest evidence on the effectiveness of telerehabilitation was for knee pain, osteoarthritis and stroke. Outcomes for remote post-surgical therapy for total-knee arthroplasty were found to be similar and—in some instances—better than in-person therapy, said AMA member Thiru Annaswamy, MD, a professor at the Pennsylvania State University College of Medicine, where he chairs the department of physical medicine and rehabilitation.
Dr. Annaswamy also noted the potential for personalizing remote rehabilitation treatment that “meets the patient where they are at.”
“There is an opportunity to improve outcomes in settings such as the home, where a patient would be encouraged to continue their rehabilitation once they're discharged from a supervised rehabilitation program and left on their own,” he explained. “There's an opportunity to improve outcomes in those settings where outcomes have traditionally plateaued.”
Telerehab is widely used
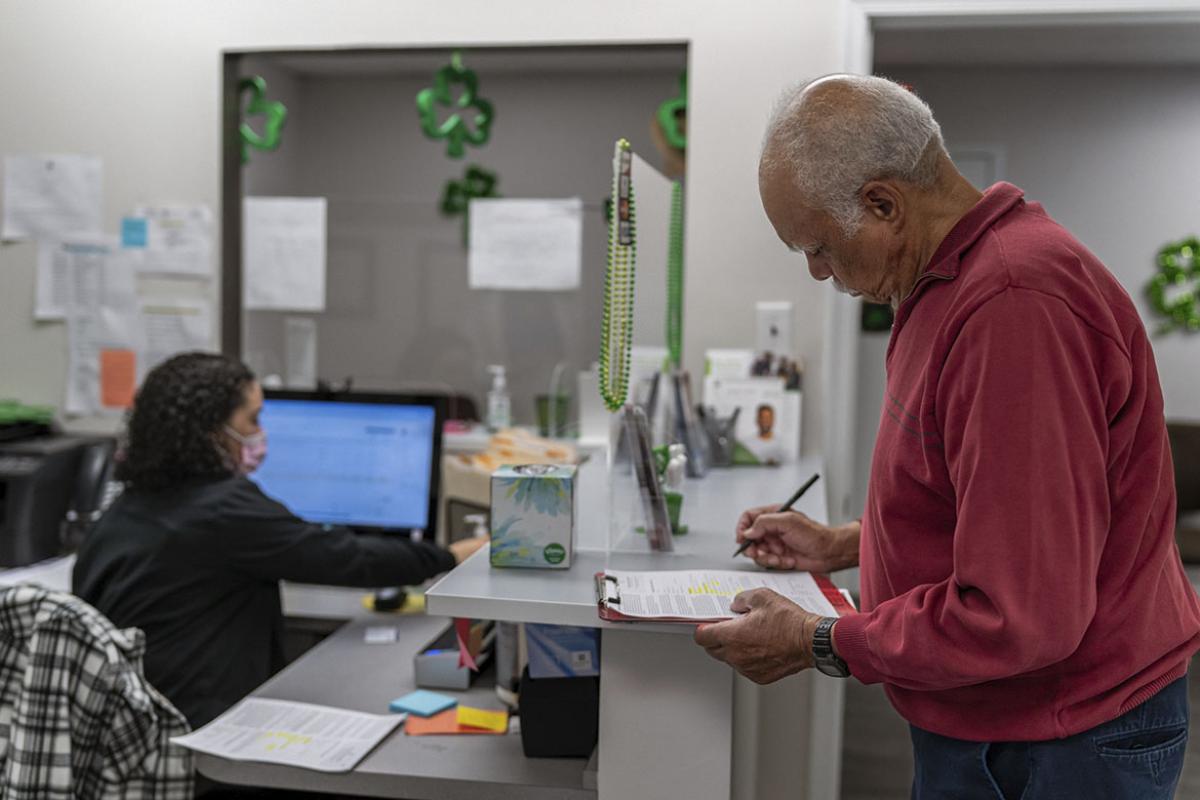
A large majority (84%) of physical medicine and rehabilitation physicians use telehealth in their practice, according to survey results discussed in the webinar.
The most common uses were for post-surgical, post-hospitalization or chronic condition follow-up care (76%), followed by screening, assessments or diagnosis (52%).
Barriers to offering telehealth services included:
- Lack of insurance coverage—77%
- Roll back of pandemic waivers, coverage and payment policies—77%.
- Low or no payment—69%.
“Technology issues” were cited by 61% of respondents, and Todd Rowland, MD, chair, of the AAPM&R Telehealth Workgroup.
“Limited digital literacy certainly has gotten better over the decades, but there are ongoing issues with folks—particularly, patients who are over 80—in terms of ability to participate,” said Dr. Rowland, an AMA member and PM&R physician for Duke Health.
“Our academy continues to encourage our members to utilize and integrate telehealth into their practice,” he added. “We're continuing to advance advocacy strategies for both payment parity, continued coverage, waiver expansions, and increased access to services.”
Visit AMA Advocacy in Action to find out what’s at stake in supporting telehealth and other advocacy priorities the AMA is actively working on.