The management of electronic health records (EHRs) has become one of the greatest administrative challenges facing physicians today. The volume of patient data is such, said one researcher, that if one were to print out all of the documentation in a single electronic patient record the result would be a stack the size of a late Hemingway novel.
“It makes it very difficult to pore through what could be 100 pages of a chart,” said Michael D. Wang, MD, a fellow in clinical informatics at the University of California, San Francisco (UCSF) Department of Medicine.
What’s more, in this age of “note bloat,” as Dr. Wang describes it, assessing what patient information is the most up-to-date and significant can also prompt considerable head-scratching: Who wrote the note? When did she write it? Why is there so much repetition? Why are there so few updates?
With these and related questions in mind, Dr. Wang and several UCSF colleagues undertook a study to look at the provenance of information contained in 23,630 UCSF physician notes written in the EHR over an eight-month period in 2016. Using tools built into their EHR, they were able to determine whether the notes had been entered manually, imported from another source—such as laboratory test results or vital signs data—or copied from other notes and then pasted.
The results of the study, documented in a recent research letter in JAMA Internal Medicine, are striking. Only 18 percent of the text in a typical patient record was original text that had been entered manually. Almost half of the text—46 percent—had been copied and pasted, while 36 percent had been imported. The differences in EHR record-keeping practices among medical students, residents and direct care hospitalists were fairly negligible, with each group copying and pasting information at least three or four times as often as they had manually entered information.
The practice of “copying or importing text increases the risk of including outdated, inaccurate or unnecessary information, which can undermine the utility of notes and lead to a clinical error,” Dr. Wang and his co-authors wrote. In making that argument, they cited a 2013 JAMA Internal Medicine article whose authors concluded that “copying and pasting mistakes … contributed to more than one-third (35.7 percent) of errors” in patients whose charts had copied notes during a study of ambulatory patient safety.
In a conversation with AMA Wire® following the publication of his research letter, Dr. Wang said that he was not against the practice of copying and pasting patient information per se, but that “judicious copying is the best policy for now.”
Given that physicians “are responsible for everything in the note,” Dr. Wang acknowledged, it will be difficult for many to refrain from copying and pasting older patient information in the EHR. However, he said, that process is a “lower-fidelity method of entering information” than writing an original entry in the EHR. He likened it to an email that has been forwarded so many times by so many people that it is challenging to locate who created the original message—and when.
The crux of the problem for the physician striving to determine the best course of treatment for her patient is this, said Dr. Wang: Was the note text from the referring physician written today or a year ago?
Dr. Wang said that technological refinements in EHR platforms should mitigate some of these concerns. Newer EHRs have tools that function like tracking mechanisms, allowing physicians to discern readily how, when and by whom information was entered.
“The whole note has a timestamp,” he said, which will preclude the time and need to suss out its source.
Should any doubt remain as to the accuracy of information in a patient’s EHR, best practices dictate that a physician identify the author of the information and confirm it with that person, said Dr. Wang.
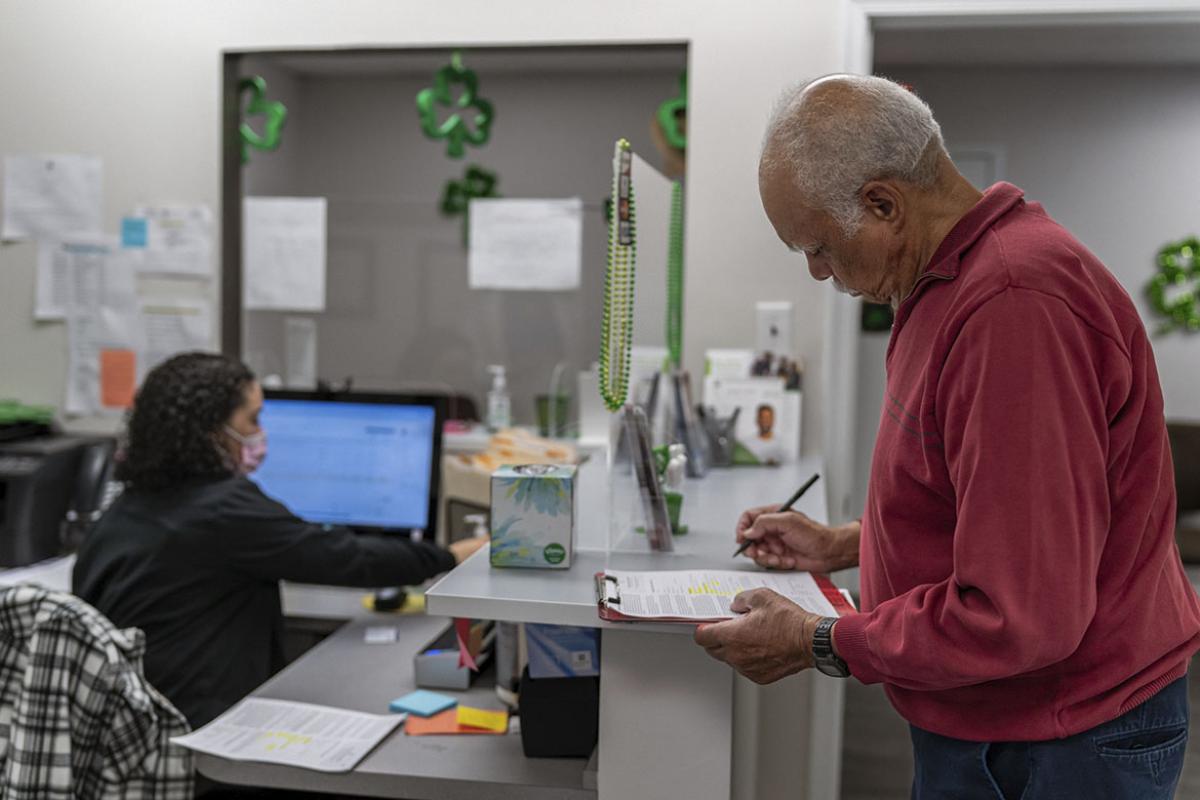
Almost one-half of the physician workday is now spent on EHR data entry and other administrative desk, work while only 27 percent is spent on direct clinical face time with patients, according to a time-motion study published in Annals of Internal Medicine last year.
Over the long haul, Dr. Wang added, physicians and policymakers will need to consider the depth and breadth of information captured in a patient profile to determine what the EHR of the future will look like. What the billing requirements or legal expectations will be are among the questions that the shapers of EHRs will need to ask and answer, he said.