It’s no secret that many physicians are unhappy with their electronic health record (EHR) systems, thanks in large part to cumbersome processes and limited features that get in the way of patient care. Now a panel of experts has called for EHR overhaul, outlining the eight top challenges and solutions for improving EHR usability for physicians and their patients.
This new framework for EHR usability—developed by the AMA and an external advisory committee of practicing physicians and health IT experts, researchers and executives—focuses on leveraging the potential of EHRs to enhance patient care, improve productivity and reduce administrative costs. Here are the eight solutions this group identified to address the biggest challenges:
Enhance physicians’ ability to provide high-quality patient care
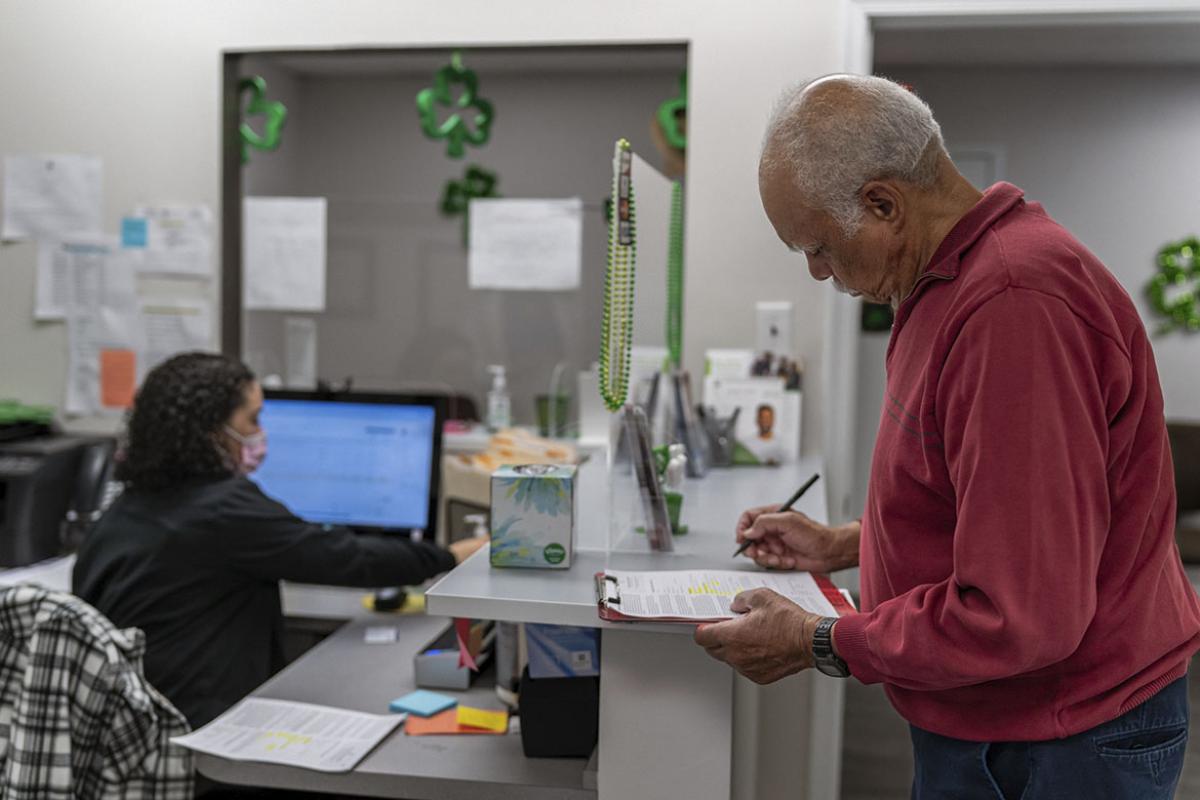
Poor EHR design gets in the way of face-to-face interaction with patients because physicians are forced to spend more time documenting required information of questionable value. Features such as pop-up reminders, cumbersome menus and poor user interfaces can make EHRs far more time consuming than paper charts.
Instead, EHRs should be designed to enable physician-patient engagement. Technology should fit seamlessly into the practice and be based on work flow needs.
Support team-based care
Current technology often requires physicians to enter data or perform tasks that other team members should be empowered to complete. EHR systems instead should be designed to maximize each person’s productivity in accordance with state licensure laws and allow physicians to delegate tasks as appropriate.
Promote care coordination
Transitioning patient care can be a challenge without full EHR interoperability and robust tracking. EHR systems need to automatically track referrals, consultations, orders and labs so physicians easily can follow the patient’s progression throughout their care.
Offer product modularity and configurability
Few EHR systems are built to accommodate physicians’ practice patterns and work flows, which vary depending on size, specialty and setting. Making EHR systems more modular would allow physicians to configure their health IT environment to best suit their work flows and patient populations. Allowing vendors to focus on specialized applications also would produce the tailored technology physicians need.
Reduce cognitive work load
Although physicians spend significant time navigating their EHR systems, many physicians say that the quality of the clinical narrative in paper charts is more succinct and reflective of the pertinent clinical information. A lack of context and overly structured data capture requirements, meanwhile, can make interpretation difficult.
EHRs need to support medical decision-making with concise, context-sensitive real-time data. To achieve this, IT developers may need to create sophisticated tools for reporting, analyzing data and supporting decisions. These tools should be customized for each practice environment.
Promote interoperability and data exchange
Data “lock in” is a common problem. EHR systems should facilitate connected health care across care settings and enable both exporting data and properly incorporating data from other systems. The end result should be a coherent longitudinal patient record that is built from various sources and can be accessed in real time.
Facilitate digital patient engagement
Most EHR systems are not designed to support digital patient engagement. But incorporating increased interoperability between EHR systems and patients’ mobile technologies and telehealth technologies would be an asset for promoting health and wellness and managing chronic illnesses.
Expedite user input into product design and post-implementation feedback
The meaningful use program requires physicians to use certified EHR technology, but many of these products have performed poorly in real-world practice settings. EHR systems should give users an automated option to provide context-sensitive feedback that is used to improve system performance and safety.
“Physicians believe it is a national imperative to reframe policy around the desired future capabilities of this technology and emphasize clinical care improvements as the primary focus,” AMA President-Elect Steven J. Stack, MD, said.
As part of its Professional Satisfaction and Practice Sustainability initiative, the AMA will use this framework to work with physicians, vendors, policymakers, health care systems and researchers to drive EHR improvements that can advance the delivery of high-quality, affordable care.
Table of Contents
- Enhance physicians’ ability to provide high-quality patient care
- Support team-based care
- Promote care coordination
- Offer product modularity and configurability
- Reduce cognitive work load
- Promote interoperability and data exchange
- Facilitate digital patient engagement
- Expedite user input into product design and post-implementation feedback