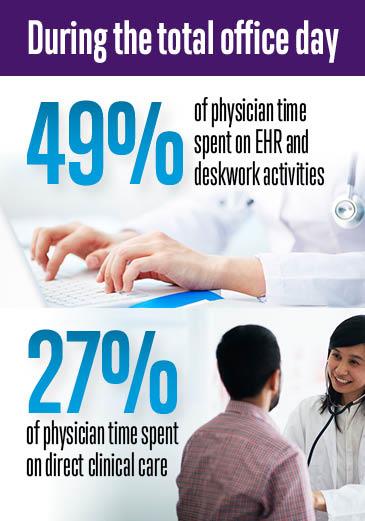
Almost one-half of the physician workday is now spent on electronic health record (EHR) data entry and other administrative desk work while only 27 percent is spent on direct clinical face time with patients, a time-motion study published Monday in the Annals of Internal Medicine found. This finding is further proof that administrative burdens are directly affecting the patient-physician relationship. Though efforts are underway to make EHRs more practical for clinical use, there are ways to relieve this burden through team-based care.
The time-motion study, conducted by experts at the AMA and Dartmouth-Hitchcock Health Care System, also found that for every hour of face-to-face time with patients, physicians spend nearly two additional hours on their EHR and other clerical desk work throughout the day.
Physicians do not feel these are the tasks that should be taking up a majority of their work day—they undercut the patient-physician relationship.
“I am not surprised to hear these results, and I can tell you no one who practices medicine today would be surprised by them,” said AMA Immediate-Past President Steven J. Stack, MD, to entrepreneurs at MATTER, Chicago’s health care technology incubator. “But they highlight exactly why new technologies that can bring greater efficiencies to medicine are so important.”
The time-motion study correlates with a study published recently in the Journal of Graduate Medical Education that tracked the average “mouse miles”—or active time—residents spent using EHRs. The study found that first-year residents spent an average of five hours per day on the EHR caring for a maximum of 10 patients.
Taking back time for patients
The importance of the patient-physician relationship is why some physicians are looking at ways to take back that stolen time. Kevin Hopkins, MD, a family physician at the Cleveland Clinic in Strongsville, Ohio, saw this happening in his practice and implemented a new team care model. “I was staring at the computer screen rather than looking at the patient,” he said. “This is one of the biggest complaints we get from patients.”
“One day I realized that if I didn’t have to do this documentation I would really like my work,” Dr. Hopkins said. So he and his team developed templates specific to their practice and patients. He taught his staff how to use health maintenance reminders in their EHR to place orders for mammography screening, labs and immunizations. They also made workplace modifications such as installing curtains to offer privacy to patients while the medical assistant remains in the exam room to document, and a computer workstation in the hallway to allow Dr. Hopkins to make minor note edits between patients.
“We have worked with the MAs to develop their multi-tasking skills,” he said. “They need to be typing, listening to me and watching what parts of the exam I am doing all at the same time. We trained them with shadowing and repetition.”
“The MAs are more fully engaged in patient care than they have ever been and they enjoy their work,” he said. “They have increased knowledge about medical care in general and about their individual patients.”
A module from the AMA’s STEPS Forward™ collection of practice improvement strategies can show you how to bring team documentation to your practice. The collection offers several modules to help physicians relieve the burden of current EHR inefficiency, including EHR software selection and purchase and EHR implementation.
Other ways to alleviate administrative burdens included in the collection are modules on how to adopt a patient pre-registration process, implement synchronized prescription renewal and expanded rooming and discharge protocols.
Findings ways to do less homework
The time-motion study also found that outside office hours, physicians spend another one to two hours of personal time each night doing clerical work—mostly related to EHRs. The findings suggest that documentation support with either dictation or documentation assistance services may increase direct clinical face time with patients.
Jim Ingram, MD, a family physician in Auburn, Ind., saw some of the same issues that Dr. Hopkins saw at the Cleveland Clinic and took action as well. He now works with two certified medical assistants (CMA). One CMA rooms the patient, then updates the problem list, the medication list, and allergies and uses EHR templates to get as much history as possible.
The CMA then leaves the room to huddle with Dr. Ingram and they review all of the information before performing the exam. This frees Dr. Ingram up to build the valuable trust that is needed for an effective patient-physician relationship. He is not staring at the computer in the exam room—he is looking at the patient.
After the exam, Dr. Ingram and the CMA step outside of the exam room and review everything that was discussed and the treatment plan. He then joins the second CMA and repeats the process with the next patient.
“I never come in on my day off or work in the evenings on notes like I used to,” he said. “I am much more relaxed during the visits and I am more thorough with my patients. I no longer have to flip through the chart looking for things or look away from the patient.”
“The biggest return on investment was achieving a real sense of teamwork, increased joy in practice and getting rid of extra work at nights,” Dr. Ingram said. “Patients are better served by me and the CMAs, and patient satisfaction has increased.”
Making EHRs interoperable, less burdensome for physicians
The time-motion study quantifies the results of an AMA study with the RAND Corporation that confirmed poorly designed EHRs and other administrative tasks have become obstacles to providing high-quality care to patients and are leading contributors to physician burnout.
Late last year, the AMA and MedStar developed a new framework to evaluate the top EHR products, said Michael L. Hodgkins, MD, AMA vice president and chief medical information officer. “And only three vendors got perfect scores.”
The EHR User-Centered Design Evaluation Framework employs a 15-point scale intended to evaluate EHR vendors’ compliance with best practices for a user-centered design process to encourage the Office of the National Coordinator for Health Information Technology to raise the bar on federal usability certification.
Also, the AMA’s grassroots campaign BreakTheRedTape.org in January held a town hall, in which physicians came together to offer solutions to what EHRs need and how they could work better for physicians and their patients.
In 2014, a panel of experts led by AMA President Steven J. Stack, MD, developed and published eight top challenges and solutions for improving EHR usability for physicians and their patients. These principles focus on leveraging the potential of EHRs to enhance patient care, improve productivity and reduce administrative costs