A physician cannot act alone in an effective health system. That point can be made by data, highlighting the importance of patient engagement on numerous levels, or by talking with and understanding the key players in shaping a health system.
A program at East Carolina University’s Brody School of Medicine is doing both, with the ultimate goal of creating physicians who can shape effective systemwide health care in the coming decades.
Faculty members from East Carolina shared the details of the Leaders in Innovative Health Care program (LINC) during a presentation at the recent AMA ChangeMedEd™ 2017 National Conference.
“In our core curriculum, students are learning how to think about health systems science competencies and how that pertains to their future practice,” said Libby Baxley, MD, senior associate dean for academic affairs at ECU. “LINC is really designed for people who will become the CMOs [chief medical officers], chief quality officers and CEOs of the future for the health systems in which they work.”
Starting early
Students can apply to be part of the LINC program following their first semester of medical school, with the program accepting up to 10 students per class. In taking students so early in the medical school journey, the idea is to get them thinking about medicine from a broader perspective at the outset.
The instruction portion of the program begins with an eight-week immersion during the summer following a student’s first year of medical training.
“The students are really engaged in learning at that time,” said Luan Lawson, MD, ECU’s assistant dean for medical education and student development. “They are looking for opportunities to expand their knowledge, they have specific interests.” Initially, Dr. Lawson said, some wondered whether the students would be ready to benefit from the material.
“But they really have blossomed,” she said. “It’s an opportunity for them to think beyond some of the foundational science components and get a much broader view of the health system from the earlier stages.”
Learning by doing
The summer curriculum focuses on a number of topics, including leadership, quality improvement, patient safety, interprofessional practice, population health and health care policy.
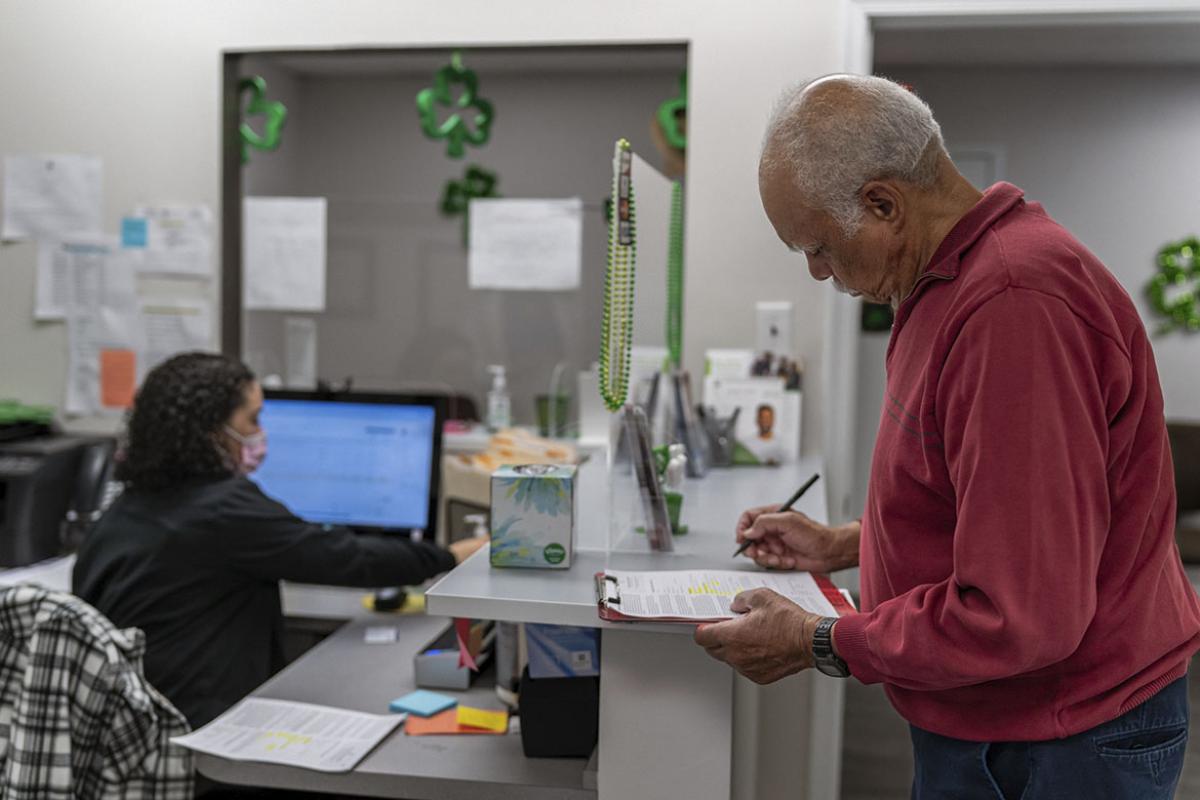
The learning plan includes delivery of foundational knowledge through online modules, readings or the typical didactic lecture component, and those lessons are all reinforced with experiential learning activities. As part of the field work, LINC students engage in meetings with the health system’s CEO and other senior administrators, as well as policy discussions with experts at the state medical society. They also shadow a patient medical visit from the moment the patient arrives in the parking lot to the time they return to the parking lot to leave, offering a detailed view of the experience from the patient’s perspective.
“While students may not have had the background experience, they certainly brought a lot of enthusiasm,” Dr. Lawson said. “But I can tell you they didn’t bring any enthusiasm for online modules or sitting in a classroom. We really tried to focus on how to build a curriculum so that they understand the foundational. But we can provide them with the experiences that they can put into practice, understand how this would relate to the clinical care they are going to provide and how to become leaders in health systems science.”
Following the summer immersion program, LINC students meet about a half dozen times per school year for continued learning sessions, in addition to participating in independent quality-improvement projects. Those meetings build toward a capstone elective in the fourth year in which students present the projects they have conducted with the guidance of a faculty mentor. Projects have focused on quality improvement initiatives such as using a software simulation to redesign staffing in the emergency department, improving pathways to reduce sepsis mortality, and implementing a standardized handoff for students in clinical rotations.
The first cohort of medical students participating in the LINC program will graduate in with the class of 2018 with their MD and and “Distinction in Health Systems Transformation and Leadership.” ECU faculty members have high hopes for these graduates’ future in medicine.
“These students will think and look differently at the system than their peers,” said Timothy Reeder, MD, director of the LINC program. “I anticipate and expect that because of their different worldview, they are going to be doing administrative roles, in a higher percentage than their peers are. But even if they are not in formal roles, they are going to be thinking about how to continuously improve their health system, their practice or whatever environment they find themselves in.”
The presentation about the LINC program was among dozens that took place during the ChangeMedEd conference. The event showcased how the AMA, through its Accelerating Change in Medical Education initiative, is working to reimagine and shape the future of medical education.
- Medical faculty get a playbook for newest role: academic coach
- Pre-clinical med students perform health data deep dives
- Population health should be a major focus in remaking med ed