PrEP, or pre-exposure prophylaxis, is a safe and effective medication that can prevent at-risk patients from contracting HIV, yet the treatment is not widely known by physicians or the patient base that could benefit most from it. Learn what HIV experts say about the treatment and the obstacles to integrating it into primary care practice.
Getting the word out
PrEP reaches a small proportion of the Americans who could benefit from it, experts said at an education session by the AMA LGBT Advisory Committee during the 2016 AMA Annual Meeting.
“What’s really interesting about it is a lot of people haven’t heard about it,” said Magda Houlberg, MD, chief clinical officer of the Howard Brown Health Center in Chicago. “You’d think people would want to shout it from the mountains.”
PrEP consists of tenofovir/emtricitabine, a once-a-day prevention option for HIV-negative men and women that reduces the risk of HIV. While the U.S. Food and Drug Administration approved PrEP in July 2012, a 2015 survey by the Centers for Disease Control and Prevention (CDC) found that 34 percent of primary care physicians and nurses had never heard of it. The CDC offers more information on PrEP at its website on HIV/AIDS.
What gets in the way of adoption
Obstacles to use remain, said panelist Noël Gordon, Jr., HIV specialist with the Human Rights Campaign. While 1.2 million Americans could benefit from the treatment, about 4 percent of them have used it, he said.
He named several factors that have slowed adoption of PrEP:
- Unawareness. Just 25 percent of gay and bisexual men have heard of PrEP, Gordon said.
- Low self-perception of risk. “I once talked to a friend and asked him what he thought his risk was, and he said low,” Gordon said. “Then I asked him if he used condoms on a regular basis, and he said no. I just can’t reconcile those two things in my mind.”
- Stigma and expense. The stigma around HIV risk is still alive despite gains, Gordon said. And while insurance coverage is widespread, many patients associate PrEP with high cost.
Dr. Houlberg has introduced about 2,000 patients to PrEP at her Chicago clinic. Howard Brown Health Center initiated 1,137 PrEP treatments in 2015, about 5 percent of the national total, according to official clinic numbers. NAM, a UK-based charity that tracks HIV/AIDS issues, reports that more than 49,000 patients in the U.S. have so far filled prescriptions for PrEP.
Panelists named groups they believed were most at risk of HIV and could benefit most from PrEP:
- Men who have sex with men
- Transgender women
- Intravenous drug users and their partners.
- Heterosexuals who have many sex partners
Gordon said those four populations remain largely unaware of HIV risks, despite efforts to educate them.
Moving it into primary care
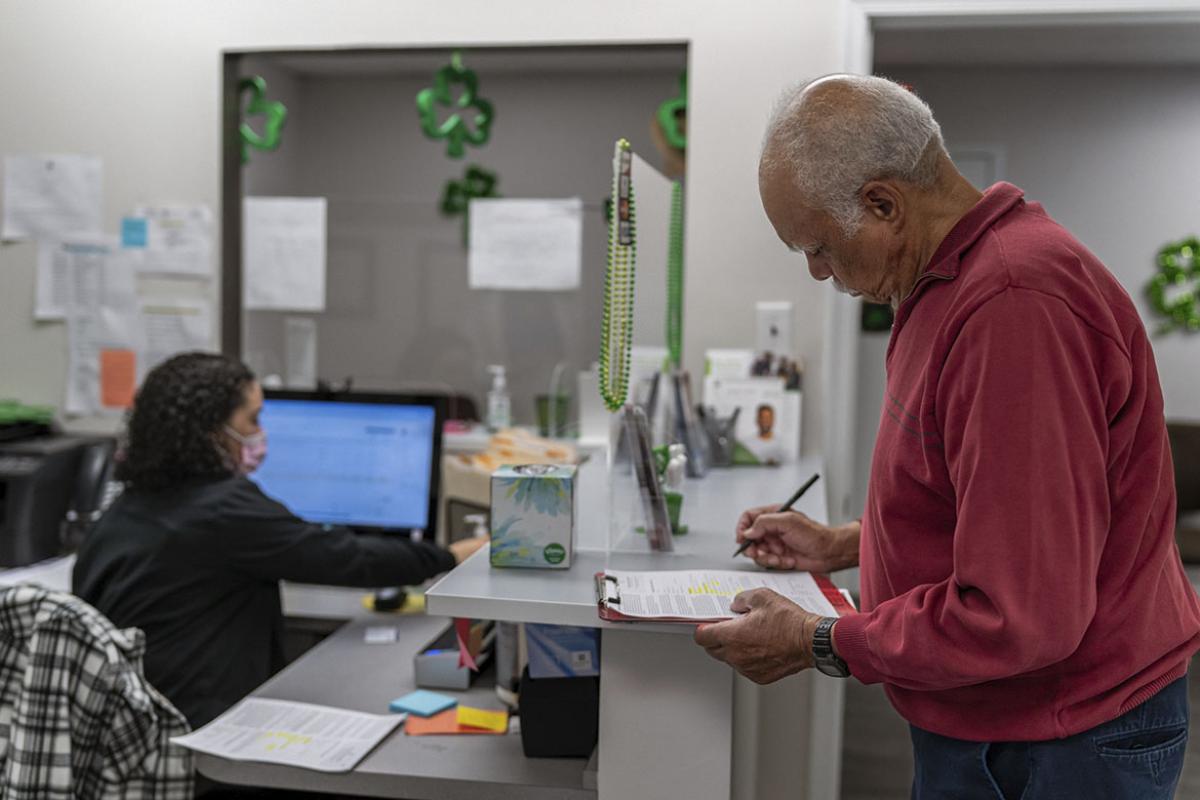
Dr. Houlberg said that in many cases PrEP treatment has served a wider purpose by providing patients with a door into the world of medical care.
“A lot of it is more like health counseling,” she said. “We’ve gotten a lot of people into preventive care overall. We see them and we can say, ‘Wow, you have high blood pressure.’ We never would have gotten that opportunity otherwise.”
Dr. Houlberg said primary care physicians often remain reluctant to adopt PrEP treatment, perhaps leery of treating a disease that has not appeared or fearful that treating PrEP patients would open the floodgates to endless monitoring, follow-ups and tests.
But she said PrEP treatment is far more trouble-free than many physicians believe, and she would like to see primary care embrace it.
“I want people to be able to access care with someone they trust, someone they’re familiar with,” she said.
Consult the Centers for Disease Control and Prevention’s guidelines for using PReP to learn more.