It’s a commonly avoided conversation about an inevitable event.
“Advance care planning conversations often do not take place because patients, family members and clinicians each wait for the other to initiate them,” the National Academy of Medicine—formerly known as the Institute of Medicine—said in its 2015 report, Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life.
To get more of those end-of-life care discussions going and make them as effective as possible, the AMA has developed training materials and ethical guidelines that together provide deep and actionable understanding into what patients want and physicians are able to provide. Also adding momentum is Medicare payment, starting in 2016, for a voluntary advance-care planning consultation with a physician or other qualified health care professional.
The AMA Code of Medical Ethics offers guidance that strongly encourages end-of-life planning and advance directives. The Code defines the physician’s role and recognizes the fundamental tenet of patient autonomy, including the patient’s right to modify a decision. The guidance addresses major issues in end-of-life care and includes support for patient decisions to withhold or withdraw life-sustaining intervention, and orders not to attempt resuscitation.
The National Academy of Medicine’s report, which runs longer than 600 pages, addresses the complex topic of end-of-life decisions in great detail, but provides a simple standard for what should be achieved in an individual basis.
“For most people, death results from one or more diseases that must be managed carefully over weeks, months or even years,” the report says. “Ideally, health care harmonizes with social, psychological, and spiritual support as the end of life approaches. To achieve this goal, care near the end of life should be person-centered, family-oriented and evidence-based.”
Physicians play a central role in that, which entails both their clinical skills and ethics by which they practice. The IOM notes, however, that in formal medical education and training there has been a “lack of attention to developing clinicians’ ability to talk effectively to patients about dying and teaching them to take the time to truly listen to patients’ expression of their concerns, values, and goals.”
A letter for the end of life
One of the most difficult things for a patient to hear, and for a physician to say, is that death is coming soon. As AMA physician education materials point out, “Very few of the nearly 2.6 million Americans who will die this year have their end-of-life decisions on file with their health care providers.” The AMA, through STEPS Forward™, helps physicians with its educational module, “Planning for End-of-Life Decisions with Your Patients.”
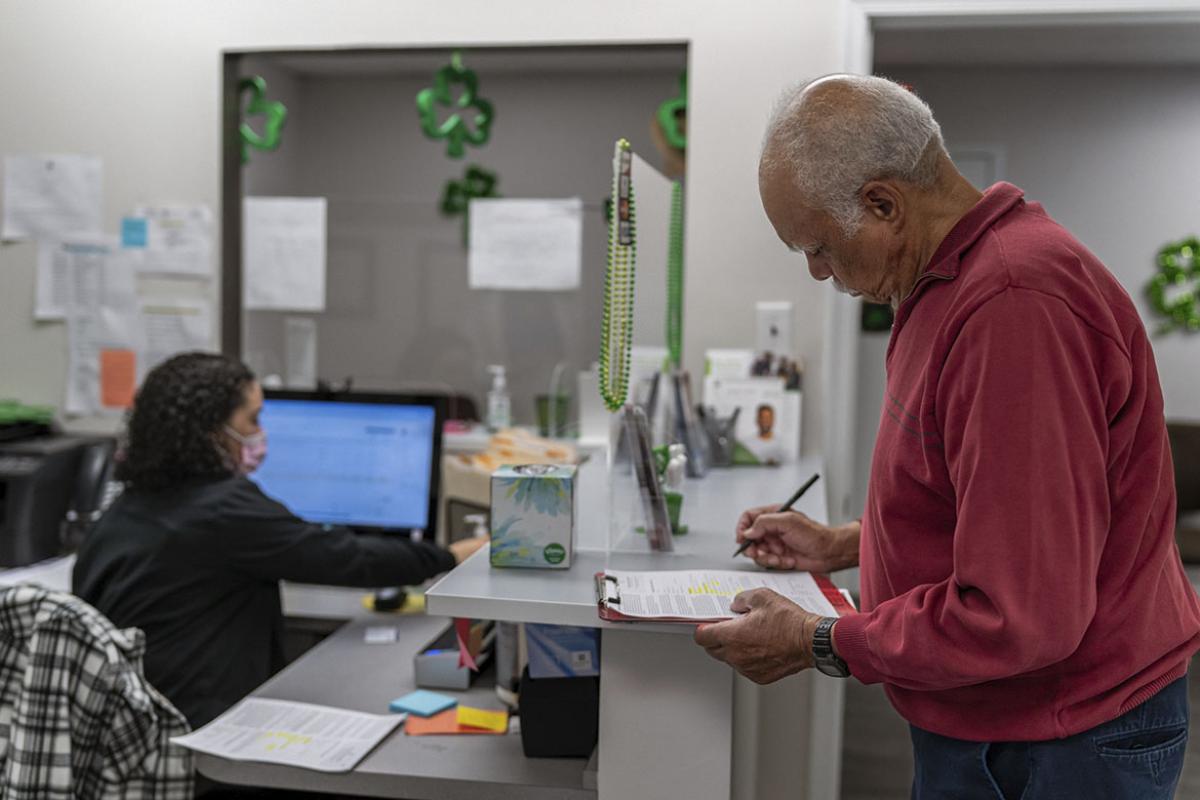
The CME credit-eligible module is built around a resource from the Stanford University Department of Medicine’s Letter Project. Patients are provided with a focused, easy-to-understand, end-of-life letter template they fill in. It covers what matters most to the patient in terms of their time remaining, specific family situations, and care instructions, including palliative sedation. Though not a formal advance directive or living will, the letter can be used as the basis for those documents and can be included in the patient’s medical record.
AMA’s STEPS Forward is an open-access platform featuring more than 50 modules that offer actionable, expert-driven strategies and insights supported by practical resources and tools. Based on best practices from the field, STEPS Forward modules empower practices to identify areas or opportunities for improvement, set meaningful and achievable goals, and implement transformative changes designed to increase operational efficiencies, elevate clinical team engagement, and improve patient care.
Several modules have been developed from the generous grant funding of the federal Transforming Clinical Practices Initiative (TCPI), an effort designed to help clinicians achieve large-scale health transformation through TCPI’s Practice Transformation Networks.
The AMA, in collaboration with TCPI, is providing technical assistance and peer-level support by way of STEPS Forward resources to enrolled practices. The AMA is also engaging the national physician community in health care transformation through network projects, change packages, success stories and training modules.