The 2018 Medicare Physician Fee Schedule proposed rule recently issued by the Centers for Medicare and Medicaid Services (CMS) includes proposals to boost coverage of diabetes prevention and telehealth services.
The CMS proposal includes “a number of positive changes that could improve patient care and save taxpayer dollars,” according to the AMA. Chief among these are a plan for expanding the Medicare Diabetes Prevention Program (MDPP), and new possibilities for telehealth services.
“The annual physician fee schedule update is a chance for CMS to modify Medicare policy to ensure the best possible treatment options for patients,” said AMA President David O. Barbe, MD (@DBarbe_MD). “The AMA is encouraged by many of the proposed changes and applauds the administration for working with the AMA to address physician concerns.”
Sept. 11 is the deadline to submit comments on the document’s proposed Medicare payment rules and policies—which includes an overall positive payment-rate update of 0.31 percent.
Diabetes Prevention Program setup
Included in the proposed rule are steps that would further implement a Medicare DPP, which the CMS describes as a structured intervention aimed at preventing a progression from prediabetes to type 2 diabetes in at-risk individuals. Previous research has shown that evidence-based lifestyle changes resulting in modest weight loss can sharply cut the rate at which people with prediabetes go on to develop type 2 diabetes.
In a news release, the AMA said it “commends” CMS for going forward to expand coverage of the DPP model the Association has helped promote among physicians and policymakers. More than a quarter of U.S. seniors have type 2 diabetes and that prevalence is expected to double by 2050 unless preventive efforts such as MDPP make headway.
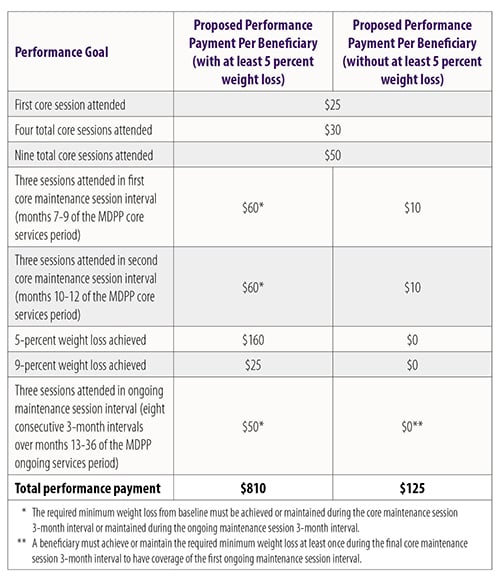
CMS proposes a “performance-based payment structure” ranging between $125 and $810 depending on participant attendance and weight loss in a three-year program consisting of 16 “core” sessions in the first six months, six “core maintenance” sessions in the next six months, followed by 24 monthly “ongoing maintenance” sessions. Payments would be updated annually to account for inflation based on the Consumer Price Index.
Strictly for comparison’s sake, CMS noted that the $810 figure would equal almost $18 a session if a fee-for-service payment mechanism had been proposed.
This would exceed the existing fee-for-service CPT code of around $10 for “education and training for patient self-management by a qualified, nonphysician health care professional.”
CMS notes that it considered linking payment to other criteria such as hemoglobin A1c levels, but post-intervention levels were not evaluated in the pilots so it was sticking with session attendance and weight loss.
The proposal is limited to three years, in part, at least, because the CMS chief actuary saw that anything longer than that was “untested.”
Telehealth services added
CMS is not proposing a DPP with all virtual sessions, though a limited number of virtual make-up sessions are allowed. The AMA is a strong supporter of online DPP because it can help meet the needs of seniors with prediabetes by providing greater access to these evidence-based programs and providing more choice for patients. The Association also offers online CME to expand your knowledge in diabetes management. Explore ways to prevent type 2 diabetes in at-risk patients, along with other content in the Practice Transformation Series.
The proposed rule includes discussion of adding and rejecting a number of new virtual or telehealth services to the Medicare Physician Fee Schedule.
Among those CMS is considering adding to the fee schedule are:
- Counseling, shared decision-making visit to discuss eligibility and need for a lung cancer screen using a low-dose CT scan.
- Assessing needs and planning care for patients requiring chronic-care management services.
- Providing 60 minutes of crisis psychotherapy, plus separate code for payment of each additional 30 minutes of service (with “the explicit condition of payment” based on the physician or health professional’s ability to mobilize resources at the patient’s site to “defuse the crisis and restore safety”).
Services CMS is proposing to keep off of the physician fee schedule include a number of physical, occupational and speech therapy services delivered predominantly by nonphysicians. It is also rejecting suggestions to add several remote evaluation and management (E&M) services for hospitalized patients.
In addition to the items discussed above, the proposed 2018 Medicare Physician Fee Schedule would change payments for hundreds of “potentially misvalued” CPT codes, alter E&M coding and documentation requirements, delay requirements to consult appropriate use criteria before ordering advanced imaging services, create new codes for opioid-use disorder treatments, and refine data collection and reporting requirements for the clinical laboratory fee schedule. Watch for additional coverage of the proposed Medicare Physician Fee Schedule in AMA Wire®.
- Final Medicare fee schedule expands DPP, boosts care coordination
- Medicare fee schedule proposed rule needs work
- Physicians work with YMCA to prevent diabetes in two more states