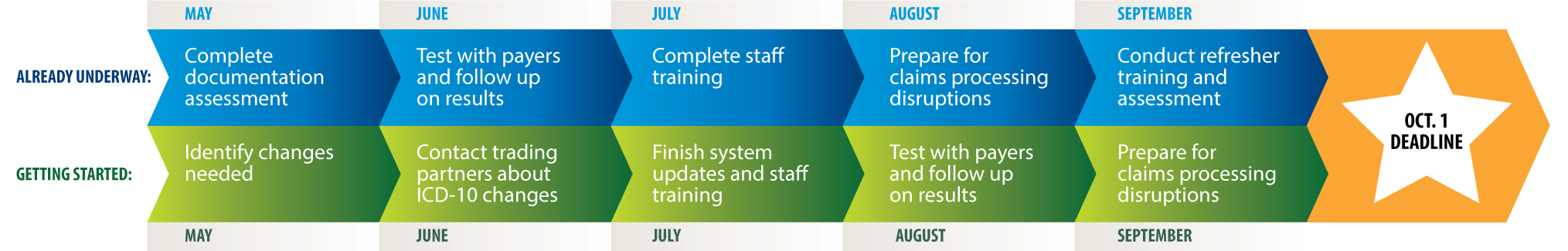
Less than 75 days remain before the Oct. 1 deadline to implement the ICD-10 code set, so make sure you’re prepping your practice. In Month Four of our ICD-10 primer, learn the next steps you should take.
What to tackle in August
Use these tips from the AMA and the Centers for Medicare & Medicaid Services’ (CMS) Road to 10 Implementation Guide to bring your practice up to speed for the new code set.
Still getting started?
If you’re still in the early stages of prepping your practice, spend the month testing your practice’s ICD-10 readiness and identify potential problems. There are different types of testing (log in), and each type serves a different purpose.
- Perform content-based testing to assess your practice’s documentation and ability to code in ICD-10. In this type of testing, your practice uses documentation to code a clinical scenario in the new code set. The Healthcare Information and Management Systems Society offers resources to help your practice with this kind of testing.
- Conduct internal testing to evaluate your practice’s ability to create and use ICD-10 codes throughout the patient work flow in place of when you currently use ICD-9 codes. This type of testing requires your practice to have system upgrades installed already and helps you follow the flow of a patient through a visit to identify the points at which codes are used. Use this testing to identify any gaps in your ICD-10 updates.
- Do external testing to test your practice’s ability to send and receive transactions that use ICD-10 codes with your external trading partners, including your billing service, clearinghouse and payers. Check with these groups about their testing plans. One type of external test is acknowledgement testing with Medicare, which simply acknowledges that a claim has been received. Physicians can perform acknowledgement testing with their Medicare Administrative Contractors and the Common Electronic Data Interchange contractor any time until the Oct. 1 implementation date.
Already on your way?
Now is the time to prepare for possible disruptions in claims processing. While the AMA has secured provisions from CMS to ease the transition to the new code set, physicians should still be ready, especially because private payers may not ease up their claims payment processes.
Make sure you have taken the most important steps to prevent cash flow interruptions. They are to ensure:
- Your systems can accommodate the ICD-10 codes
- Your staff is trained
- You have tested thoroughly with your trading partners
If you’ve been following a solid transition plan, you should be well-prepared to handle any potential claims disruptions. Learn what else your practice can do to prepare financially for ICD-10.
The provisions the AMA secured from CMS address claims denials, quality reporting penalties, payment disruptions and navigating transition problems. Read more about the changes at AMA Wire®.
For even more help, get the AMA’s must-have ICD-10 resources and read the rest of the posts in this monthly series.