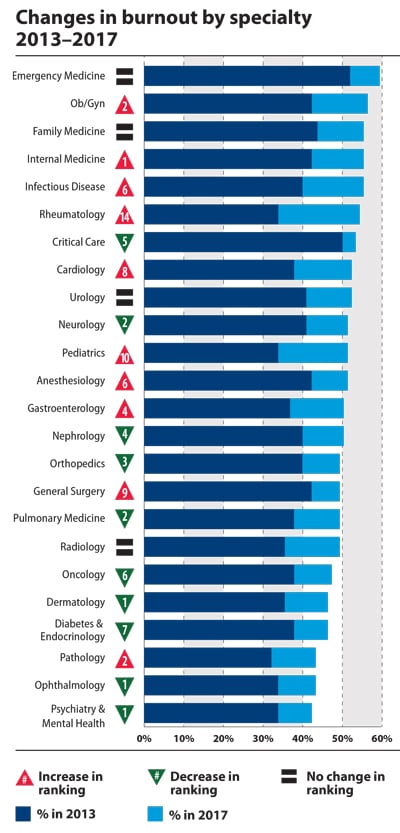
Physicians from 27 specialties graded the severity of their burnout on a scale of one to seven in a recent Medscape survey—one being that it does not interfere, and seven indicating thoughts of leaving medicine. All but one specialty selected a four or higher. The most affected specialty? Emergency medicine, with nearly 60 percent of ED physicians saying they feel burned out, up from half in 2013. How can the rising prevalence and severity of burnout be addressed? Regulatory, systemic and practice environment issues appear to be key.
Too many bureaucratic tasks, spending too many hours at work, feeling like just a cog in a wheel, increased computerization of practice: In the “Medscape Lifestyle Report 2017,” more than 14,000 physicians surveyed designated these four concerns as the top causes of burnout.
“Today’s medical practice environment is destroying the altruism and commitment of our physicians,” said Tait Shanafelt, MD, a hematologist and physician-burnout researcher at the Mayo Clinic, in a presentation at a NEJM Catalyst event last June. “We need to stop blaming individuals and treat physician burnout as a system issue … If it affects half our physicians, it is indirectly affecting half our patients.”
Dr. Shanafelt delivered a presentation that same month at the 2016 AMA Annual Meeting in Chicago, where he examined this scenario: “If I told you we had a system issue that affected quality of care, limited access to care, and eroded patient satisfaction … you would immediately assign a team of systems engineers, physicians, administrators at your center to fix that problem rapidly.”
And burnout is a system issue just like that, Dr. Shanafelt said. In order to address the issue, the focus should be on changing the practice environment and the system, but “we have not mobilized the way we would to address other factors affecting quality, access and patient satisfaction,” he said.
In 2013, the first year of the “Medscape Lifestyle Report,” emergency medicine had the highest rates of burnout at just over 50 percent. That specialty, in 2017, is now close to 60 percent. Meanwhile, on the severity scale urology landed in the uncoveted top spot with a 4.6 rating. That compares with a 4.2 burnout severity rating for emergency medicine. Infectious disease medicine physicians rated their burnout severity lowest, at 3.9 on the seven-point scale. Yet, over the four years between reports, infectious disease medicine burnout rates rose 15 percentage points to make that specialty the fifth highest in share of physician burnout.
For infectious disease medicine, it is hard to ignore the two pandemics that arose. First, Ebola entered the global sphere in 2014 and put pressure on infectious disease specialists, and it was almost immediately followed by the Zika virus.
Rheumatology also saw a big jump in burnout. While about one-third of rheumatologists reported burnout in 2013, more than half scored as burned out in the 2017 edition of the Medscape report. Pediatrics, cardiology and general surgery also saw increases in burnout over the years. No specialty reported less burnout.
When the types of issues identified by physicians in this report get in the way of a physician’s ability to provide care to a patient, burnout symptoms may present. “[Burnout] primarily relates to your professional spirit of life, and it primarily affects individuals whose work involves an intense interaction with people,” Dr. Shanafelt said.
The question then arises whether physician burnout differs from the general working population. The AMA and the Mayo Clinic provided an answer in a recent study published in Mayo Clinic Proceedings. Compared with the general U.S. population, physicians worked a median of 10 hours more per week, displayed higher rates of emotional exhaustion and reported lower satisfaction with work-life balance, the study found.
Though the general U.S. population does experience burnout, the current state of the health care system is clearly driving increases in physician burnout at a higher rate.
Organizations can make positive changes
One practice in Minneapolis, not far from the Mayo Clinic, found a simple solution to provide their physicians and staff a space to “reset.” Hennepin County Medical Center, through their Office for Professional Worklife, gathers volunteers from each department to discuss the best ways the organization can address physician burnout.
One of their ideas was to create a “reset room” where physicians and other health professionals can retreat if they need a moment to recover from a traumatic event or just to get away for a moment. And this is just one of several ways Hennepin is helping their physicians.
A reset room is very much in line with Dr. Shanafelt’s recommendation that, in order to address burnout properly, the solutions have to be numerous, yet organizations and physicians alike must recognize that those fixes will not solve physician burnout overnight. They should be directed at giving physicians the skill set to “navigate the choppy water,” he said, with the understanding that the organization needs to do its part to mitigate the systemic and environmental issues that cause burnout.
Electronic health record (EHR) systems are among these systemic issues. Almost one-half of the physician work day is spent on EHR data entry and other administrative desk work, according to a recent time-motion study conducted by the AMA and Dartmouth-Hitchcock Health Care System. Only 27 percent of a physician’s time is spent on direct clinical care, the study points out.
Another key finding in the study is that for every hour of face-to-face time with patients, physicians spend nearly two additional hours on their EHR and clerical desk work.
Physicians entered medicine to help patients. Anything that is getting in the way of patient care, whether it is systemic or environmental, should be the focus of change.
If you have conducted research on physician health and wellness, the American Conference on Physician Health™, which takes place Sept. 28 – 29 in San Francisco, is open for presentation submissions. Review the submission guidelines and email your abstract proposal to [email protected].