If you are preparing for the United States Medical Licensing Examination® (USMLE®) Step 1 exam, you might want to know which questions are most often missed by test-prep takers. Check out this example from Kaplan Medical, and read an expert explanation of the answer. Also check out all posts in this series.
This month’s stumper
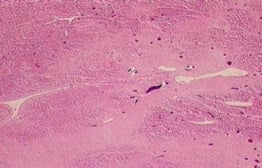
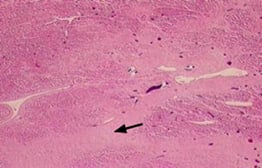
A 58-year-old woman with a history of hypertension and hyperlipidemia comes to the physician five weeks after an anterior wall myocardial infarction. The patient reports worsening shortness of breath and fatigue. A physical examination reveals bi-basilar crackles on auscultation of the lung fields. After admission, the patient's condition deteriorates, and she eventually succumbs to her illness. An autopsy is performed and a photomicrograph of myocardial tissue is shown.
Which of the following cardiac abnormalities is most likely responsible for this patient's death?
A. Coronary artery aneurysm.
B. Interventricular septal rupture.
C. Left ventricular free wall rupture.
D. Left ventricular free wall rupture.
E. Ventricular aneurysm.
The correct answer is E.
Kaplan Medical explains why
Several weeks after myocardial infarction (MI), a thin fibrous scar (black arrow in image below) is found in lieu of the lost myocardial tissue. The thin scar has diminished resistance to wall tension associated with developing high intraventricular pressure, causing it to bulge out during systole and progressively expand into a ventricular aneurysm. Ventricular aneurysms are more likely to develop after large anterior transmural infarctions.
Our patient presents with classic symptoms (dyspnea) and signs (bibasilar lung crackles) of left-sided congestive heart failure (CHF), which is the most common cause of death in patients with ventricular aneurysms.
CHF results from akinesis (poor contractility of scarred myocardium) or dyskinesis (paradoxical ballooning during systolic contraction) of the aneurysm, resulting in diminished stroke volume. Other complications include ventricular arrhythmias and mural thrombosis.
Patients may also present with ventricular pseudoaneurysms, where an imminent cardiac rupture is contained by fragile scar tissue. There is no myocardium or endocardium in a pseudoaneurysm (unlike in a true aneurysm), only scar tissue. Urgent surgery is required in these cases due to high probability of cardiac rupture and mortality.
Why the other answers are wrong
It is important to note that several complications (septal rupture, free wall rupture, papillary muscle rupture) occur near the five-day post-MI window. This period is characterized by macrophage clearing of necrotic tissue and early granulation tissue formation in the infarcted region of myocardium. Granulation tissue contains weak type III collagen versus the stronger type I collagen found in later scar tissue. As a result, this is a vulnerable period with the potential for the complications listed below.
Choice A, coronary artery aneurysm:
- Congenital abnormality of the coronary arteries.
- Acquired forms are associated with Kawasaki disease.
- May eventually result in MI.
Choice B, interventricular septal rupture is a feared complication of MIs:
- Five to seven days after an infarction of the left anterior descending artery.
- Hypotension, heart failure, and new holosystolic murmur.
Choice C, left ventricular free wall rupture sudden cardiac death:
- Five to seven days post-MI, most common in left ventricle.
- Microscopic: hemorrhage, macrophages, fibroblasts, new vessel formation (not seen in the autopsy section above).
- Leads to hemopericardium and cardiac tamponade rather than CHF.
Choice D: papillary muscle rupture:
- Two to seven days post-MI.
- Acute severe mitral regurgitation → pulmonary edema and hypotension.
- Most commonly rupture of posteromedial papillary muscle, due to sole blood supply from the posterior descending artery (anterolateral papillary muscle has a dual blood supply).
The AMA and Kaplan have teamed up to support you in reaching your goal of passing the USMLE® or COMLEX-USA®. If you're looking for additional resources, Kaplan provides free access to tools for pre-clinical studies, including Kaplan’s Lecture Notes series, Integrated Vignettes, Shelf Prep and more.
For more prep questions on USMLE Steps 1, 2 and 3, view other posts in this series. .