If you’re preparing for the United States Medical Licensing Examination (USMLE) Step 1 exam, you might want to know which questions are most often missed by test-prep takers. Check out this example from Kaplan Medical, and read an expert explanation of the answer. Also check out all posts in this series.
This month’s stumper
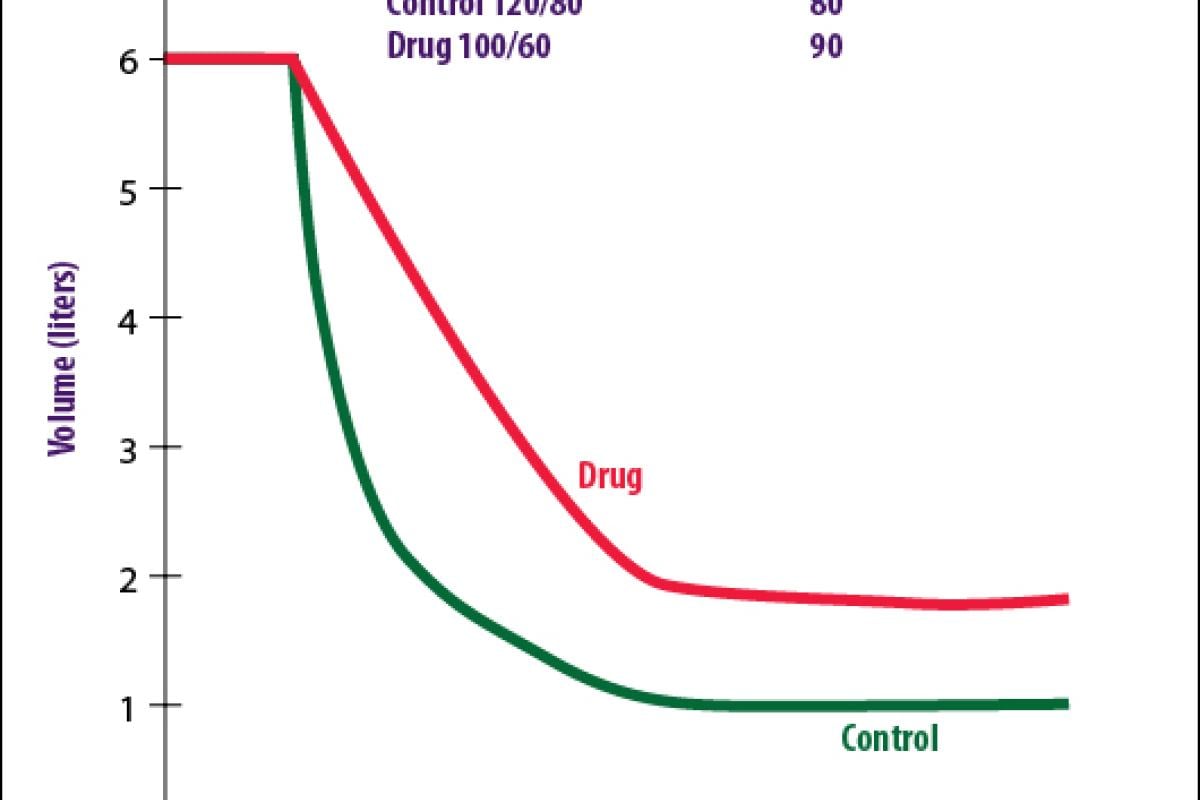
A patient undergoing pulmonary function testing is asked to inspire maximally and then exhale as hard as possible while a spirometer measures forced expiratory volume in one second (FEV1), total volume, and forced vital capacity (FVC) (the curve labeled "Control" above). Normally, FEV1 is about 80 percent of FVC. After the patient inhales an unknown drug, a second recording is taken (the curve labeled "Drug" above). The effects of the drug on blood pressure and heart rate are also noted.
Stimulation of which of the following receptor types is responsible for the change in FVC?
A. Alpha-1 adrenergic.
B. Beta-1 adrenergic.
C. Beta-2 adrenergic.
D. Muscarinic-2 cholinergic.
E. Muscarinic-3 cholinergic.
The correct answer is E.
Kaplan Medical explains why
The control values for the pulmonary function test are FVC = 5.0, FEV1 = 4, and FEV1/FVC = 80 percent. After the drug is given, all of these values are decreased, indicating obstructive symptoms. Stimulation of bronchiolar smooth-muscle M3 receptors causes bronchoconstriction and produces these results. In addition, stimulation of non-innervated vascular M3 receptors results in vasodilation and a drop in blood pressure. As a result of the baroreceptor reflex, heart rate is increased.
Why the other answers are wrong
Choice A: There are no alpha-adrenergic receptors on bronchiolar smooth muscle. In addition, stimulation of vascular alpha-adrenergic receptors results in an increase in blood pressure and a baroreceptor-mediated decrease in heart rate.
Choice B: Beta-1 adrenergic receptors are also not found on bronchiolar smooth muscle. These receptors are found primarily on the heart and juxtaglomerular cells in the afferent arteriole. Stimulation of these receptors increases blood pressure and heart rate.
Choice C: Stimulation of beta-2 adrenergic receptors causes bronchodilation, which would tend to increase rather than decrease FEV1 and FVC on the pulmonary function test. However, stimulation of these receptors on blood vessels causes a drop in blood pressure and a rise in heart rate.
Choice D: M2 receptors are found predominantly on the heart and would not cause any change in pulmonary function tests. Stimulation would produce a decrease in heart rate with little change in blood pressure.
Tips to remember
- In the lungs, stimulation of M3 receptors produces bronchoconstriction and increases mucus secretion, whereas stimulation of beta-2 receptors produces bronchodilation.
- On the other hand, whenever a blood vessel is directly stimulated it will generate a baroreceptor reflex aimed to counteract the effect exerted by the drug.
- For example, M3 and beta-2 stimulation decrease blood pressure and generate a reflex tachycardia, whereas alpha-1 stimulation increases blood pressure and generates a reflex bradycardia.
The AMA and Kaplan have teamed up to support you in reaching your goal of passing the USMLE® or COMLEX-USA®. If you're looking for additional resources, Kaplan provides free access to tools for pre-clinical studies, including Kaplan’s Lecture Notes series, Integrated Vignettes, Shelf Prep and more.
For more prep questions on USMLE Steps 1, 2 and 3, view other posts in this series.