The results of a landmark duty-hours trial are in, and the findings indicate that allowing general surgery residents to work flexible, less restrictive hours improves continuity of care. While residents generally had more positive perceptions of their training, there were some personal trade-offs.
The FIRST Trial
Results of the highly anticipated Flexibility in Duty Hour Requirements for Surgical Trainees Trial, commonly known as the FIRST Trial, were recently published in the New England Journal of Medicine. This national, cluster-randomized trial involved 117 general surgery residency programs and 151 affiliated hospitals during the 2014-2015 academic year. Fifty-nine residency programs and their 71 affiliated hospitals followed standard Accreditation Council for Graduate Medical Education (ACGME) duty-hour policies, while 58 programs and their 80 affiliated hospitals followed a flexible duty-hour policy.
The study is the first large-scale, national study to examine the impact of ACGME duty-hour reforms established to prevent residents from fatigue-related errors. Residents and their mentors have been eager for data on the topic after some have raised concerns that the limits could undermine the goals of surgical training if residents are unable to follow patients through critical aspects of their care.
Under the flexible-hours policy, which included the ability to work longer shifts and take less time off between shifts than allowed under current duty-hour requirements, residents were better able to see patients through to the end of their episodes of care.
An “important finding in our study was that residents in the flexible-policy group were about half as likely to leave or miss an operation or hand-off in an active patient care issue than were those in the standard-policy group,” study authors wrote. “This suggests that the flexible, less-restrictive duty hours had their intended effect of improving continuity of care.”
Some learning environment pros; some personal life cons
Being able to stay with patients through an operation or hand-off may have contributed to residents in the flexible-policy group reporting a less negative perception of the impact that duty-hour policies had on the learning environment than residents in the standard duty-hours group.
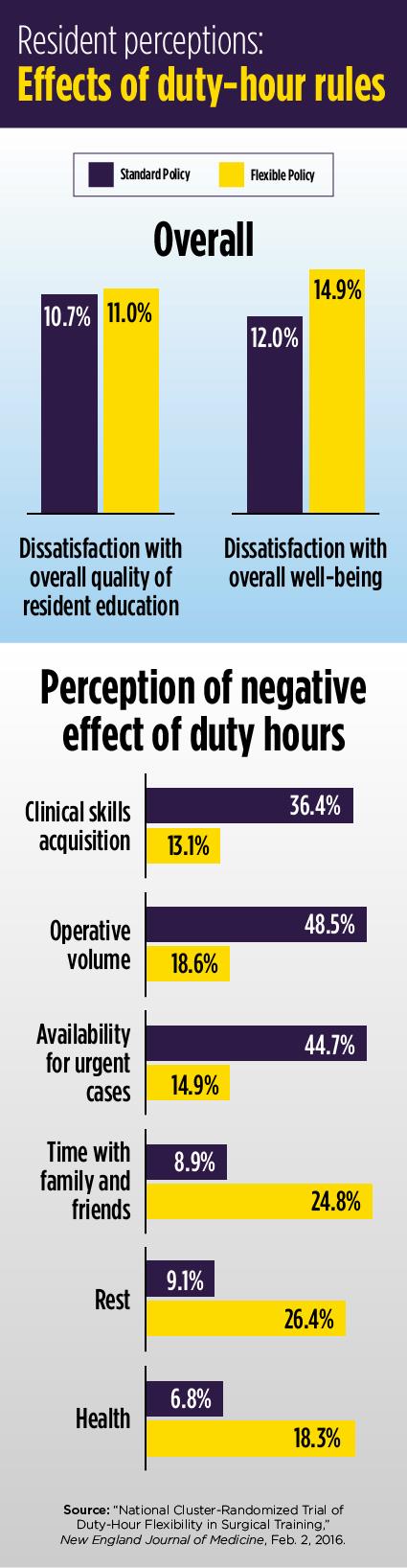
For example, when it came to learning clinical skills, 36.4 percent of residents in the standard-policy group believed duty-hour rules had a negative impact on learning, while just 13.1 percent in the flexible-group felt that way. About 49 percent of residents working under the standard duty-hour rules said they had a negative impact on learning operative skills. In comparison, 18.9 percent of residents working under the flexible duty hour-rules perceived a negative impact.
The trade-off seems to be on residents’ time away from the hospital. Residents in the flexible-policy group were more likely to report that duty hours had a negative impact on their personal lives. About 25 percent of those who worked more flexible hours reported that duty hours had a negative impact on time with family and friends, extracurricular activities, rest and health. Among those who worked the standard hours, just under 10 percent said duty hours had a negative impact on those areas.
Despite differences on specific questions, residents in both groups reported similar satisfaction rates with their overall quality of education and their overall well-being. In the standard-policy group, 10.7 percent reported being dissatisfied with the overall quality of their resident education; 11 percent in the flexible-policy group reported being dissatisfied. When it came to overall well-being, 12 percent of standard-policy residents were dissatisfied, and 14.9 percent of flexible-policy residents were dissatisfied.
Patient safety differences were negligible
Data from more than 138,000 patients showed that the less restrictive policies did not significantly increase the rate of death or serious complications for patients. The rate was 9.1 percent for the flexible-policy group and 9 percent for the standard-policy group. The similarity in rates held steady whether the surgery was emergency or elective and whether it was an outpatient or inpatient setting, study authors reported.
The FIRST trial is one of two large, multi-national resident trials that are expected to answer questions about duty-hour rules.