Conceptually understanding the potential hazards in a hospital room and being able to spot them are different skill sets. By focusing on situational awareness, the “patient safety room of horrors”—a safety-focused simulation—aims to help medical students and residents identify potential hospital room mishaps before they happen.
The room of horrors is used at the University of Chicago Pritzker School of Medicine(U. of C.), a member of the AMA Accelerating Change in Medical Education Consortium.
“When you walk into a patient's room, it's not just the medications, but many things that can put your patient at risk for some reason or other, resulting in either near-miss or adverse event,” said Jeanne Farnan, MD, MHPE, associate professor of medicine and associate dean of evaluation and continuous quality improvement at U. of C. “We try to make our residents and students very vigilant about recognizing that by stressing the importance of situational awareness.”
This teaching tool is used for preclinical medical students during their second year, and then reintroduced to them once they complete their third-year clerkships. It is also part of U. of C.’s residency training boot camp experience prior to beginning practice.
A Chicago Ideas Week lab at the MATTER offices gave visitors from all walks of life a chance to see whether they could identify the room’s hazards as part of a patient-safety boot camp. The event was made possible by the U. of C. and the Center for Healthcare Delivery Sciences and Innovation, with funding from the AMA Accelerating Change in Medical Education Consortium.
Prior to entering the room of horrors, students are given a mock door chart that details the patient’s condition. They then have 15 minutes to identify all the safety hazards surrounding the patient.
What’s wrong with these pictures?
So what are the horrors that medical students and residents may find in this hazardous hospital room? The pictures below may offer some insight.
But first, for context, here are a few key notes from patient’s chart:
- The patient is Michael Washington, a 55-year-old male with pneumonia and C. diff diarrhea.
- His hospital course has been complicated by delirium and he suffered a fall without significant injury last night.
- The patient is allergic to latex and penicillin analogues.
Keep your guard up
Research indicates that hospitals, due to the unfamiliar environment and a number of additional factors, increase the risk of a fall. That already proved to be the case for Washington, who fell during his stay. The fact that the safety railing on his hospital bed is not in use presents an opportunity for harm.
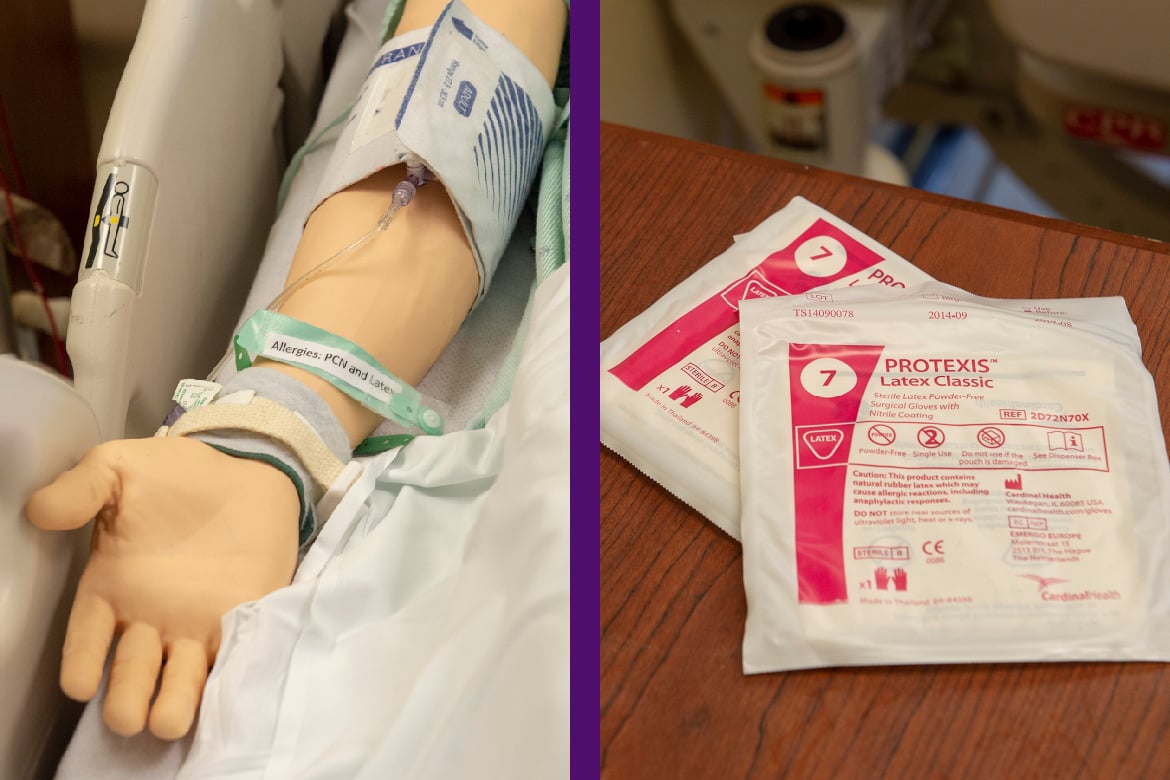
Staying mindful of allergies
Both the patient’s bracelet and chart indicate that he is allergic to latex and penicillin. Yet examining the bedside table reveals that there are latex gloves within feet of his hospital bed, and reviewing his medications demonstrates that he is receiving a penicillin analogue.
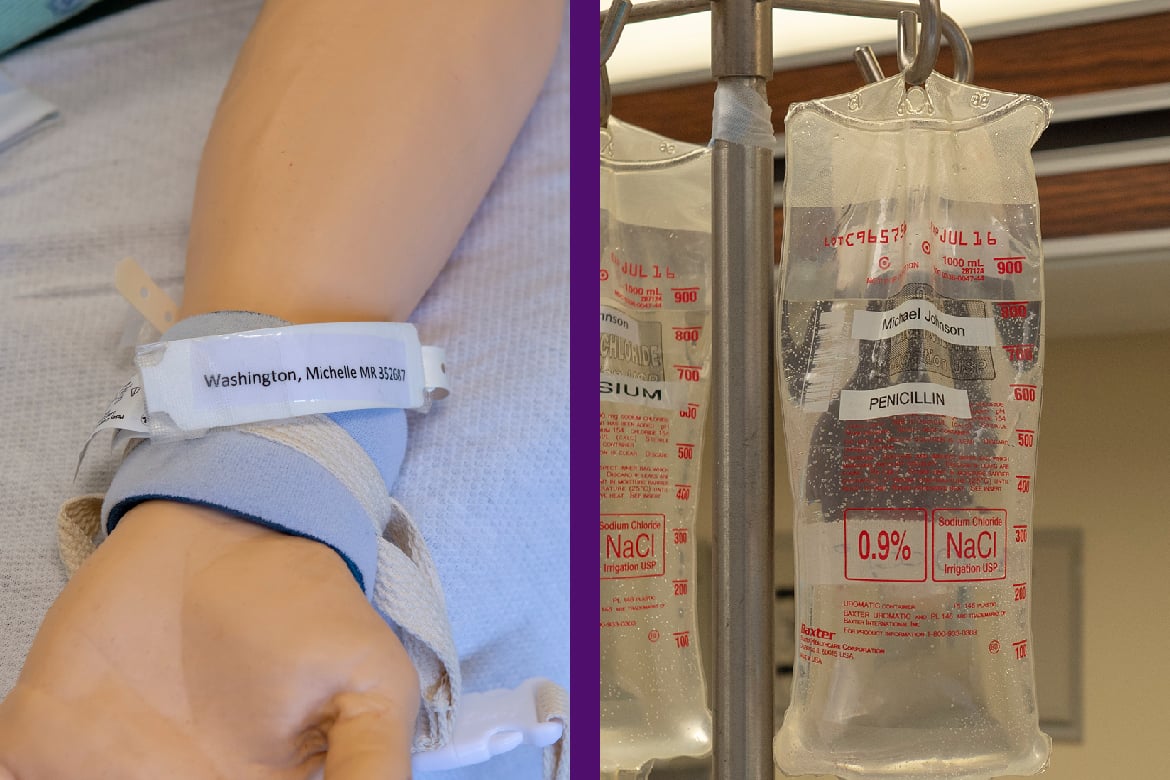
What’s in a name?
The patient’s chart and identification bracelet indicate his name is Michael Washington. A quick check of the IV pole, however, reveals that the penicillin and magnesium the patient is receiving are intended for Michael Johnson and his name is listed incorrectly on his identification bracelet.
Dirty hands, ugly results
The empty Purell dispenser in the room is a a red flag. Making it easy for physicians, other health professionals and patients to practice proper hand hygiene can go a long way toward cutting the risk of hospital-acquired infections.
What’s the cost?
In addition to safety hazards, trainees are asked to identify “cost hazards.” That value-centric approach is a response to a call for greater focus on training cost-consciousness and overuse, particularly in residency. This hypothetical patient’s cost hazards include a superfluous catheter and unnecessary hand restraints.
Dr. Farnan co-wrote a 2015 BMJ article reporting results involving 86 third-year medical students. While 83 percent of students identified the fall risk, other risks were often missed. For example, only 13 percent of the med students spotted the absence of deep venous thrombosis prophylaxis and only 5 percent correctly identified the simulated patients’ risk of pressure ulcers.
The 128 interns who completed the room of horrors were able to spot an average of 5.1 hazards out of nine, Dr. Farnan and her colleagues reported.