Overdoses and deaths related to heroin and other opioids continue to climb in Maryland, but state physicians will have opportunities to learn what they can do to reverse these trends at a series of special training programs.
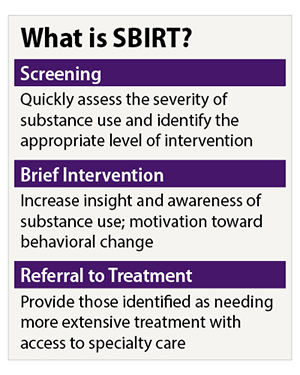
The programs are being facilitated by the Maryland State Medical Society (MedChi) and include training on how to use the Screening, Brief Intervention and Referral to Treatment (SBIRT) strategy in office-based settings and how to make better use of the state’s prescription drug-monitoring program (PDMP).
The first session was held May 24 at Doctors Community Hospital in Lanham and another was held in early June. Two more are scheduled: June 20 and June 22. MedChi CEO Gene Ransom said the goal is get 250 physicians to attend. Registration is free for the educational sessions, which feature Maryland addiction-medicine specialists.
“One of our roles is education outreach,” Ransom says. “The idea is to prescribe people the appropriate amount when opioids are necessary and that people use them [opioids] appropriately, and to also not leave any behind or in the medicine cabinet. It’s also to be able to better identify a patient who has a problem and needs help.”
Prescriptions down, overdoses up
There are about five heroin-related deaths a day in Maryland, Ransom says. Heroin-related overdose deaths increased 72 percent and fatal opioid-related overdoses increased 17 percent in the first nine months of last year compared with the same period in 2015, he added
There were 13.3 percent fewer opioid prescriptions filled in Maryland during 2016 compared with 2013, according to research done by QuintilesIMS. While this lags behind a 14.6 percent national decline in opioid prescriptions during this period, Maryland physicians had already been below the national average in terms of average opioid prescriptions per capita.
Ransom said MedChi has hired staff to contact all Maryland physicians registered with Drug Enforcement Administration to prescribe controlled substances and encourage them to enroll in the state’s prescription drug-monitoring program.
MedChi has an opioid task force started by its president-elect, Gary Pushkin, MD, a Baltimore-based orthopedic surgeon in practice for 35 years. Dr. Pushkin says he received little training in opioid prescribing beyond being told to give patients enough medication so that they wouldn’t call over the weekend.
“I want to keep our doctors out of trouble and get them the tools and education they need to do the right thing,” Dr. Pushkin says.
Maryland gets more support for treatment
Maryland Gov. Larry Hogan signed two AMA-supported bills—the Heroin and Opioid Prevent Effort (HOPE) and Treatment Act of 2017 and the Start Talking Maryland Act—May 25.
AMA Board Chair Patrice Harris, MD, said in a statement that the AMA supported the bills’ provisions for new treatment centers, increased resources for behavioral health and community health services, and enhancement of Maryland drug courts.
“We also support the increased emphasis on youth education to help our children and young adults understand the risks of opioid misuse and illicit drug use,” Dr. Harris said. “There is a long way to go to reverse the opioid epidemic—and the AMA and the nation’s physicians accept the responsibility to take steps to do so.”
Dr. Pushkin and Ransom said MedChi also strongly supported the bills, though they were disappointed that the final version of the legislation only allowed for the creation of one treatment center.
“The piece that’s missing is access to treatment,” Ransom says.
Dr. Pushkin noted that, when overdose patients show up in a hospital emergency department, they need to have their addiction treated right away.
“We can’t send them home with a phone number or put them on a two- to three-week waiting list,” he said. “We have to get them in a program right away.”
And while MedChi supported this legislation, there have been other proposals they have opposed, such as restricting patients to seven-day prescriptions.
“For a senior citizen who just had total-joint-replacement surgery, to expect them to come in one week later is just cruel,” Dr. Pushkin said.
Other solutions Dr. Pushkin believes are necessary to reverse the opioid crisis include lowering insurance co-pays on opioid alternatives such as Lidocaine patches, and making PDMP databases easier to use and having their information accessible across state lines.
“There are so many parts to this,” he said.
$10 million question
Baltimore Health Commissioner Leana Wen, MD, echoed Dr. Pushkin’s last point, noting that when she was an emergency physician in Washington, she saw patients that had also sought care in Maryland and Virginia.
Dr. Wen called MedChi one of her department’s “key partners” in addressing opioid addiction and misuse, and she applauded its promotion of the SBIRT strategy which she said has been implemented in the emergency departments of Baltimore hospitals.
“We have to prevent opioid overprescribing and increase access to treatment,” she said, adding that it was important that the legislature has “recognized that addiction is a disease that can be treated.”
Maryland was appropriated $10 million to use for opioid treatments in the federal 21st Century Cures Act.
“The most important thing to recognize for the disease of opioid addiction is that the research is there, the evidence is plenty—treatment exists and recovery is possible,” Dr. Wen said. “We don’t need more studies. We know what works. We need the resources to address the epidemic.”
The AMA Opioid Task Force has been working to increase access to naloxone, the life-saving opioid overdose antidote, increase access to MAT for patients struggling with substance-use disorderss, encourage physicians to register for and use PDMPs, reduce the stigma of substance-use disorder, educate patients and physicians on the matter, and promote safe storage and disposal of opioids and all medications.
The task force recently issued a report on physicians’ progress in efforts to reverse the nation’s opioid epidemic. Among other things, the report found that:
- PDMPs were checked 136.1 million times in 2016, a 121 percent rise from 2014.
- 118,550 physicians completed courses on opioid prescribing, pain management, addiction and related areas offered by state and medical specialty societies in 2015–2016.
- There are now more than 37,000 physicians nationwide who are certified to provide office-based MAT for opioid-use disorders.
To find out more about the AMA's efforts in this vital area, visit the End the Opioid Epidemic website.